-
- Find Care
-
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
-
-
-
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
- Participate in Research
-
- Contact us
-
- For Innovators
- Commercialization Guide for Innovators
-
-
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Getting Started
- New to Mass General Brigham
- International Patient Services
- What Is Patient Gateway?
- Planning Your Visit
- Find a Doctor (opens link in new tab)
- Appointments
- Patient Resources
- Health & Wellness
- Flu, COVID-19, & RSV
- Billing & Insurance
- Financial Assistance
- Medicare and MassHealth ACOs
- Participate in Research
- Educational Resources
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
- Find Care
-
- Overview
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
-
- Overview
- Participate in Research
-
- Overview
- About Innovation
- About
- Team
- News
- For Industry
- Venture Capital and Investments
- World Medical Innovation Forum (opens link in new tab)
- Featured Licensing Opportunities
- For Innovators
- Commercialization Guide for Innovators
- Contact us
-
- Overview
- Information for Researchers
- Compliance Office
- Research Cores
- Clinical Trials
- Advisory Services
- Featured Research
- Two Centuries of Breakthroughs
- Advances in Motion (opens link in new tab)
- Brigham on a Mission (opens link in new tab)
- Gene and Cell Therapy Institute
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Residency & fellowship programs
- Brigham and Women's Hospital
- Massachusetts General Hospital
- Mass Eye and Ear
- Newton-Wellesley Hospital
- Salem Hospital
- Integrated Mass General Brigham Programs
- Centers of Expertise
- Global & Community Health
- Health Policy & Management
- Healthcare Quality & Patient Safey
- Medical Education
- For trainees
- Prospective trainees
- Incoming trainees
- Current trainees
- Continuing Professional Development
Why Is Colorectal Cancer Increasing in Young Adults?

The incidence of young onset colorectal cancer is rising globally. A 2024 American Cancer Society report confirms colorectal cancer is now the leading cause of cancer deaths in men younger than age 50 in the United States. It’s also the second deadliest cancer among women of that same age group, behind breast cancer.
Aparna Parikh, MD, medical director of the Center for Young Adult Colorectal Cancer at Mass General Cancer Center, describes what may be driving this increase. She reviews common risk factors, current screening guidelines, and offers prevention tips.
“Colorectal cancer is largely preventable and, in most cases curable, especially if it’s detected early,” Dr. Parikh says.
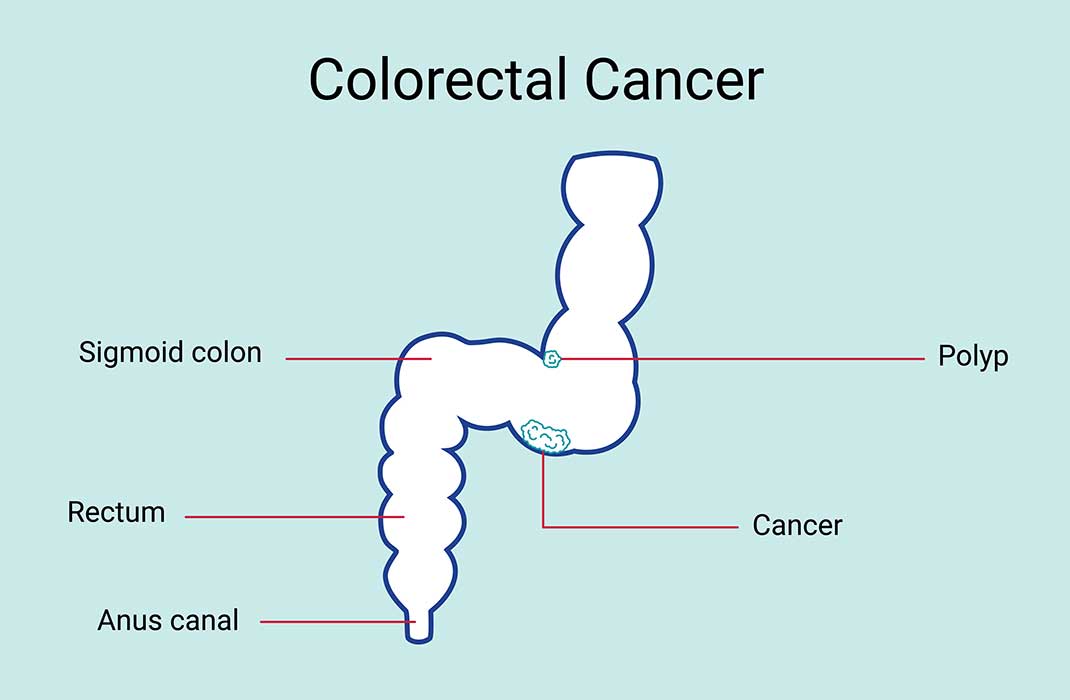
What is colorectal cancer?
What causes colorectal cancer?
Colorectal cancer occurs when there are changes in your genetic material (DNA) called mutations. Doctors often don’t know the exact cause of the genetic changes that lead to colorectal cancer. But certain genetic changes that raise your risk for colorectal cancer are passed down in families. They’re inherited, meaning that you’re born with them.
Black people have an increased risk of colorectal cancer and death from colorectal cancer compared to other races. Your lifestyle and environment also can affect your risk of colorectal cancer.
Why are more young adults getting colorectal cancer?
Your risk of having colorectal cancer increases as you age. But more and more young adults are getting colorectal cancer than in the past.
“This is active area of investigation as to why this trend is happening in younger patients,” explains Dr. Parikh. “There are many hypotheses regarding early childhood dietary or environmental exposures, along with weight changes, among others.”
Colorectal cancer risk factors
Anyone can get colorectal cancer, but certain factors make you more likely to develop it than other people. Risk factors for colorectal cancer include:
Having a personal or family history of colorectal cancer, or having a genetic syndrome. Up to 30% of all colorectal cancer diagnoses occur in patients that have a family history of colorectal cancer. People with familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary non-polyposis colorectal cancer) are more likely to develop colorectal cancer.
Having a history of adenomas. Adenomas are colorectal polyps that look abnormal under a microscope, or are 1 centimeter or larger. They can sometimes turn into cancer over time.
Having chronic ulcerative colitis or Crohn’s disease for 8 years or more.
Smoking cigarettes. Tobacco use disorder is one kind of substance use disorder (SUD).
Having three or more alcoholic drinks per day. Alcohol use disorder (AUD) and binge drinking rates in women increased during the pandemic.
Having obesity. Your doctor can calculate your body mass index (BMI) using a formula involving height and weight. If you have a BMI over 30, you have obesity.
What are colorectal cancer symptoms in young adults?
Different people have different symptoms of colorectal cancer. Some people may not have any signs or symptoms at all. Colorectal cancer symptoms may include:
Abdominal or belly discomfort or cramping
Bleeding from your rectum or finding blood in your stool
Changes in the way your stool looks or how often you move your bowels
Diarrhea, constipation, or a feeling that you can’t completely empty your bowels
Increased gas
Unexplained weight loss
It’s important to remember that these symptoms can be attributed to things that are not related to colorectal cancer. If you experience any of these symptoms, please talk to your primary care provider (PCP).
Colorectal cancer screening
It’s important to understand and follow the screening recommendations for colonoscopies. Colonoscopies can detect cancer before you have symptoms or advanced disease. Early detection is critical. It’s important to advocate for your own health and wellbeing if you have any concerning symptoms.
If you have a family history of colorectal cancer, you should get your first colonoscopy at 40 years old, or 10 years prior to when your immediate family member was diagnosed. All others should start screening at age 45, including those without symptoms.
There are other screening options, including stool-based tests, but it is important to talk to your PCP about the pros and cons of different types of screenings.
“As an oncologist who sees largely young patients, my bias is to screen earlier. But we have to be mindful of continuing to lower the screening age and considering the population-level implications,” says Dr. Parikh. “Ideally, we start to understand the drivers, and which younger individuals may be prone to develop colorectal cancer, in order to offer early screening to the right patients. A biomarker to identify risk would help us understand who to screen early. Many of my patients are in their 20s and 30s. Expanding the screening-eligible age may be a good space for stool and blood-based screening, along with risk stratification, to get the right people to colonoscopies efficiently.”
It's important to note that these other screening methods are only for patients without symptoms. If you have symptoms, it’s important to get a colonoscopy.
Colorectal cancer prevention