-
- Find Care
-
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
-
-
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
- Participate in Research
-
- Contact us
-
- For Innovators
- Commercialization Guide for Innovators
-
-
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Getting Started
- New to Mass General Brigham
- International Patient Care
- What Is Patient Gateway?
- Planning Your Visit
- Find a Doctor (opens link in new tab)
- Appointments
- Patient Resources
- Health & Wellness
- Flu, COVID-19, & RSV
- Billing & Insurance
- Financial Assistance
- Medicare and MassHealth ACOs
- Participate in Research
- Educational Resources
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
- Find Care
-
- Overview
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
-
- Overview
- Participate in Research
-
- Overview
- About Innovation
- About
- Team
- News
- For Industry
- Venture Capital and Investments
- World Medical Innovation Forum (opens link in new tab)
- Featured Licensing Opportunities
- For Innovators
- Commercialization Guide for Innovators
- Contact us
-
- Overview
- Information for Researchers
- Compliance Office
- Research Cores
- Clinical Trials
- Advisory Services
- Featured Research
- Two Centuries of Breakthroughs
- Advances in Motion (opens link in new tab)
- Brigham on a Mission (opens link in new tab)
- Gene and Cell Therapy Institute
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Residency & fellowship programs
- Brigham and Women's Hospital
- Massachusetts General Hospital
- Mass Eye and Ear
- Newton-Wellesley Hospital
- Salem Hospital
- Integrated Mass General Brigham Programs
- Centers of Expertise
- Global & Community Health
- Health Policy & Management
- Healthcare Quality & Patient Safey
- Medical Education
- For trainees
- Prospective trainees
- Incoming trainees
- Current trainees
- Continuing Professional Development
IUD Insertion Pain Relief: What You Need to Know

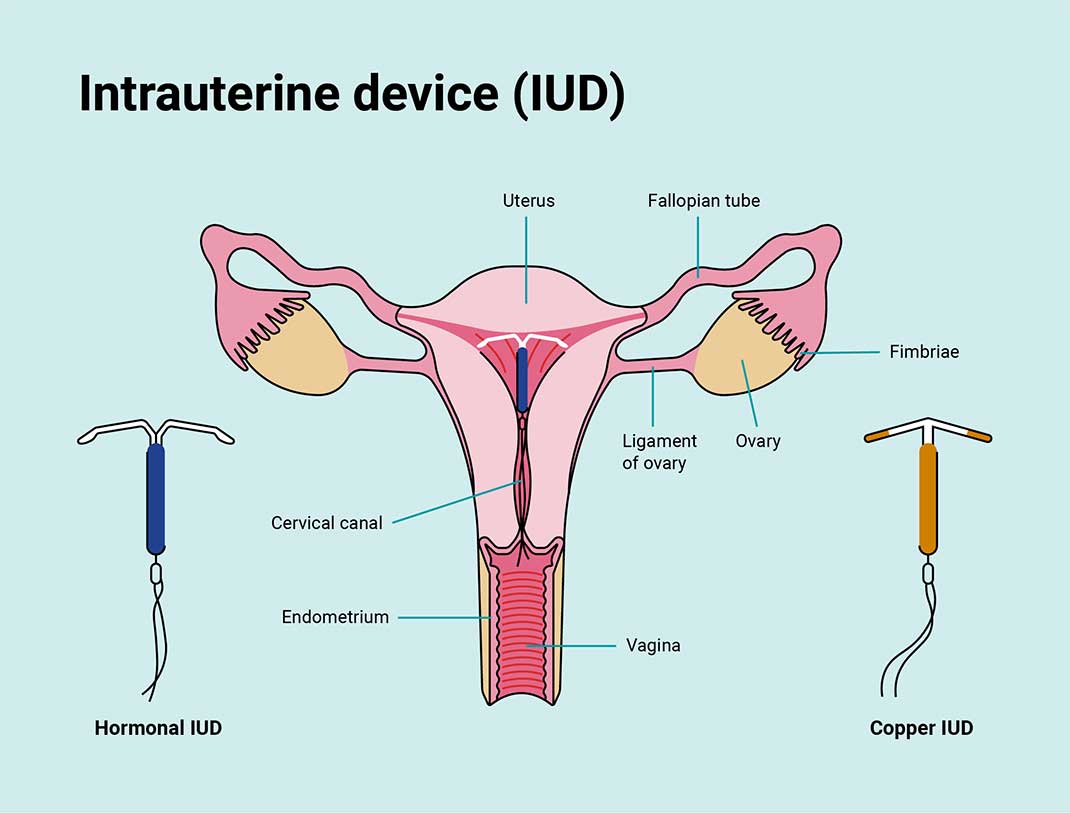
Intrauterine devices, or IUDs, are becoming increasingly popular choices for long-term birth control. This creates an opportunity for patients and clinicians to have improved dialogue about the discomfort associated with IUD insertion and options for pain management.
Most IUD insertions are done within the clinic, with the help of oral medications like ibuprofen or acetaminophen. These oral medications can decrease discomfort throughout the IUD insertion process because they get in the blood stream and affect the whole body. However, some patients want or need additional options to help alleviate the discomfort of IUD insertions.
“Despite what people might be seeing on social media, many patients do very well with IUD insertion,” says Deborah Bartz, MD, MPH, a Mass General Brigham obstetrician-gynecologist. “But pain – especially women’s pain – has been underrecognized and minimized by the medical community.”
In response to growing calls for more transparency around IUD insertion and pain, the Centers for Disease Control and Prevention (CDC) released new recommendations for providers to counsel patients on pain management options before the procedure.
“The CDC’s recommendation is that we have more open, elaborate conversations with patients about their pain,” says Dr. Bartz, who cares for patients at Brigham and Women’s Hospital. “I agree 100% with that recommendation. Hopefully it will change clinical practice to allow physicians to have those conversations, and for patients to feel more empowered to initiate those conversations.”
What are IUDs?
IUD pain relief
The CDC now recommends providers have more transparent conversations about the potential discomfort or pain associated with IUD insertion. If you’re considering getting an IUD, you and your doctor should discuss the pain management options that are available to you.
Depending on the clinic, pain relief options for IUD insertion may include:
Oral pain medication, like ibuprofen
Lidocaine spray or gel in the cervix
Para-cervical block or lidocaine injection in the cervix
Sedation
Dr. Bartz explains that there’s some uncertainty if these pain relief options make patients feel better overall. Lidocaine injections can create discomfort on their own, as doctors insert them into the cervix with a needle.
The CDC’s new recommendation included 6 studies that compared patients who received additional pain relief for IUD insertion to those that did not. Half of those studies showed patients benefited from pain relief, and the other half showed there was no benefit.
“It takes a conversation with the patient with regards to what their priorities and values are. Some patients feel very strongly about getting an injection of lidocaine, others feel strongly against it,” says Dr. Bartz.
IUD insertion and anxiety
Because of the growing conversation around IUD insertion pain, some people may be hesitant to get an IUD.
Dr. Bartz says some of that has to do with a “negativity bias” that many contraception methods fall victim to. In everyday conversations and on social media, people are more likely to talk about the negative things that are affecting them. “We're not prone to talk about things we’re not actively thinking about,” Dr. Bartz explains. “If something is going well, like if you don't have to think about your birth control, then you won't necessarily bring it up in conversation.”
Patients who are anxious about the insertion and what it will feel like can have a more negative experience. Talking about IUD insertion with your doctor beforehand can help reduce some of that anxiety.
“Treating someone's anxiety can have a direct result on their perception of pain during an IUD insertion,” she says. “A lot of patients who come in with anxiety surrounding the discomfort of the insertion often tell me after that it was easier than they expected.”
Side effects of IUDs
Dr. Bartz notes that IUDs typically have fewer side effects compared to other forms of birth control. This is largely because the device is placed directly where your reproductive organs are. Other birth controls, like the pill or shot, can cause more widespread effects throughout your body.
Your body may take some time getting used to your IUD, so any negative side effects typically go away after the first few months of having it. Side effects of an IUD may include:
Cramping or back pain for a few days after the IUD is put in
Irregular periods
Spotting between periods
Heavier or longer periods, and worse cramping during your period (typically only with copper IUDs)
If you have concerns about potential side effects, talk to your doctor. They may be able to give you more personalized advice about which IUD is right for you, and how to manage any side effects you might experience.
Have open conversations with your doctor.
If you’re interested in getting an IUD but hesitant because of concerns about pain, Dr. Bartz recommends making an appointment to talk to your provider. “Express that hesitancy and talk very deliberately about what options that clinic offers.”
The new recommendations from the CDC are an important step toward having more open and honest discussions about pain between doctors and patients. You’ll likely have a much better experience if you fully understand your options and ask questions to make informed decisions about your care.
“Being in the clinic is not the time to be the pleaser, or trying to be a ‘good patient’ out of fear of inconveniencing anybody,” says Dr. Bartz. “Patients should feel empowered and be forthcoming about what they're thinking and what they're nervous about.”