Atrial septal defect, or ASD, is serious if left untreated or undiagnosed. However, with the proper diagnosis and treatment, someone with ASD can expect to live a normal life.
-
- Find Care
-
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
-
-
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
- Participate in Research
-
- Contact us
-
- For Innovators
- Commercialization Guide for Innovators
-
-
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Getting Started
- New to Mass General Brigham
- International Patient Services
- What Is Patient Gateway?
- Planning Your Visit
- Find a Doctor (opens link in new tab)
- Appointments
- Patient Resources
- Health & Wellness
- Flu, COVID-19, & RSV
- Billing & Insurance
- Financial Assistance
- Medicare and MassHealth ACOs
- Participate in Research
- Educational Resources
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
- Find Care
-
- Overview
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
-
- Overview
- Participate in Research
-
- Overview
- About Innovation
- About
- Team
- News
- For Industry
- Venture Capital and Investments
- World Medical Innovation Forum (opens link in new tab)
- Featured Licensing Opportunities
- For Innovators
- Commercialization Guide for Innovators
- Contact us
-
- Overview
- Information for Researchers
- Compliance Office
- Research Cores
- Clinical Trials
- Advisory Services
- Featured Research
- Two Centuries of Breakthroughs
- Advances in Motion (opens link in new tab)
- Brigham on a Mission (opens link in new tab)
- Gene and Cell Therapy Institute
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Residency & fellowship programs
- Brigham and Women's Hospital
- Massachusetts General Hospital
- Mass Eye and Ear
- Newton-Wellesley Hospital
- Salem Hospital
- Integrated Mass General Brigham Programs
- Centers of Expertise
- Global & Community Health
- Health Policy & Management
- Healthcare Quality & Patient Safey
- Medical Education
- For trainees
- Prospective trainees
- Incoming trainees
- Current trainees
- Continuing Professional Development
- Patient Care
- Services and Specialties
- Heart and Vascular
- Conditions & Treatments
- Atrial Septal Defect
What is atrial septal defect?
Atrial septal defect (ASD) is often called hole in the heart. It's a condition where the septum, the wall separating the two upper chambers in the heart (the atria), has a hole or opening. The hole can cause oxygen-rich blood from the left atria to leak into the oxygen-poor blood of the right atria. When this occurs, too much blood is pumped into the lung arteries, causing the lungs and heart to work harder.
ASDs can occur at different places along the septum, and the size of the opening can vary. In most cases, when diagnosed and treated, there are few complications from ASD.
What are atrial septal defect symptoms?
Hole in heart symptoms can be tough to spot in babies, and it’s possible not to experience any symptoms until adulthood. Signs and symptoms of ASD for both children and adults include:
- Tiring easily during activity or playing
- Fatigue
- Sweating
- Shortness of breath
- Rapid breathing
- Frequent respiratory illness
- Swollen legs, feet, or abdomen
- Heart murmur
- Slow growth (in children)
Request an appointment with the heart specialists at Mass General Brigham for diagnosis and treatment options.
What are the causes of atrial septal defect?
ASD is a congenital heart defect, which means someone is born with the condition. It's possible to inherit the condition, or it can occur without any family history.
The exact cause of ASD is still unknown. Other than genetics, factors during pregnancy, like medications, alcohol and nicotine use, and environmental exposures, could potentially play a role in the development of ASD.
What are the types of atrial septal defect?
There are four main types of ASD. The type of ASD depends largely on where the actual hole or opening is located along the septum.
This is the most common type of ASD, occurring in about two-thirds of those diagnosed with the condition. The opening is located within the center of the septum separating the two atria walls.
This form of ASD occurs when there is an opening in the atrioventricular canal, which is in the lower part of the atrial septum. An opening occurs when the septum primum does not fuse with the heart chamber walls.
This type of ASD occurs when the superior vena cava and right atrium join together. The pulmonary veins are abnormal and drain to the right atrium rather than the left atrium.
The rarest type is coronary sinus ASD. Because the hole is located in the coronary sinus wall, it passes the blood from the left atrium through the heart vein to the right atrium.
How is atrial septal defect diagnosed?
Atrial septal defect is often detected during pregnancy or soon after the baby is born. However, you can be diagnosed with ASD later in life. Numerous exams can diagnose this heart condition, starting with an exam from the physician and listening to the heart through a stethoscope. An ASD murmur may be detected first, which calls for further testing.
Echocardiography, chest X-ray, computed tomography (CT), and cardiac magnetic resonance imaging (MRI) are commonly used to diagnose ASD. An electrocardiogram (an ECG or EKG) can also detect the electrical activity within the heart and an irregular heartbeat or ASD murmur.
How is atrial septal defect treated?
Atrial septal defect treatment varies widely and depends on the size and location of the hole or opening. The presence of other congenital heart defects or chronic conditions, such as severe pulmonary hypertension, could impact the course of treatment.
It is possible for the hole to close up on its own, which means treatment may not be needed. Closure can occur spontaneously when the opening is less than 5 mm and often happens before the first birthday. Even without a closure, a cardiologist may only want to monitor the opening over time, and no treatment may be required.
Nonsurgical and surgical treatments are available for ASD. A doctor may also prescribe anticoagulants and beta-blockers to control the atrial septal defect symptoms, such as an irregular heartbeat. There are specific types of ASD where surgery is the only option, or else the symptoms can worsen, causing long-term health problems.
Our heart specialists at Mass General Brigham can diagnose and compose a treatment plan for atrial septal defect and other heart conditions best suited for your individual needs.
Cardiac catheterization is commonly performed for the treatment of ASD. It can be used on both children and adults. This is where a thin, flexible tube is inserted into a blood vessel that leads to the heart. A plug is then passed through the catheter to fill the hole in the heart. The heart tissue will grow around the plug, closing the hole. Only certain types of ASD qualify for this nonsurgical treatment.
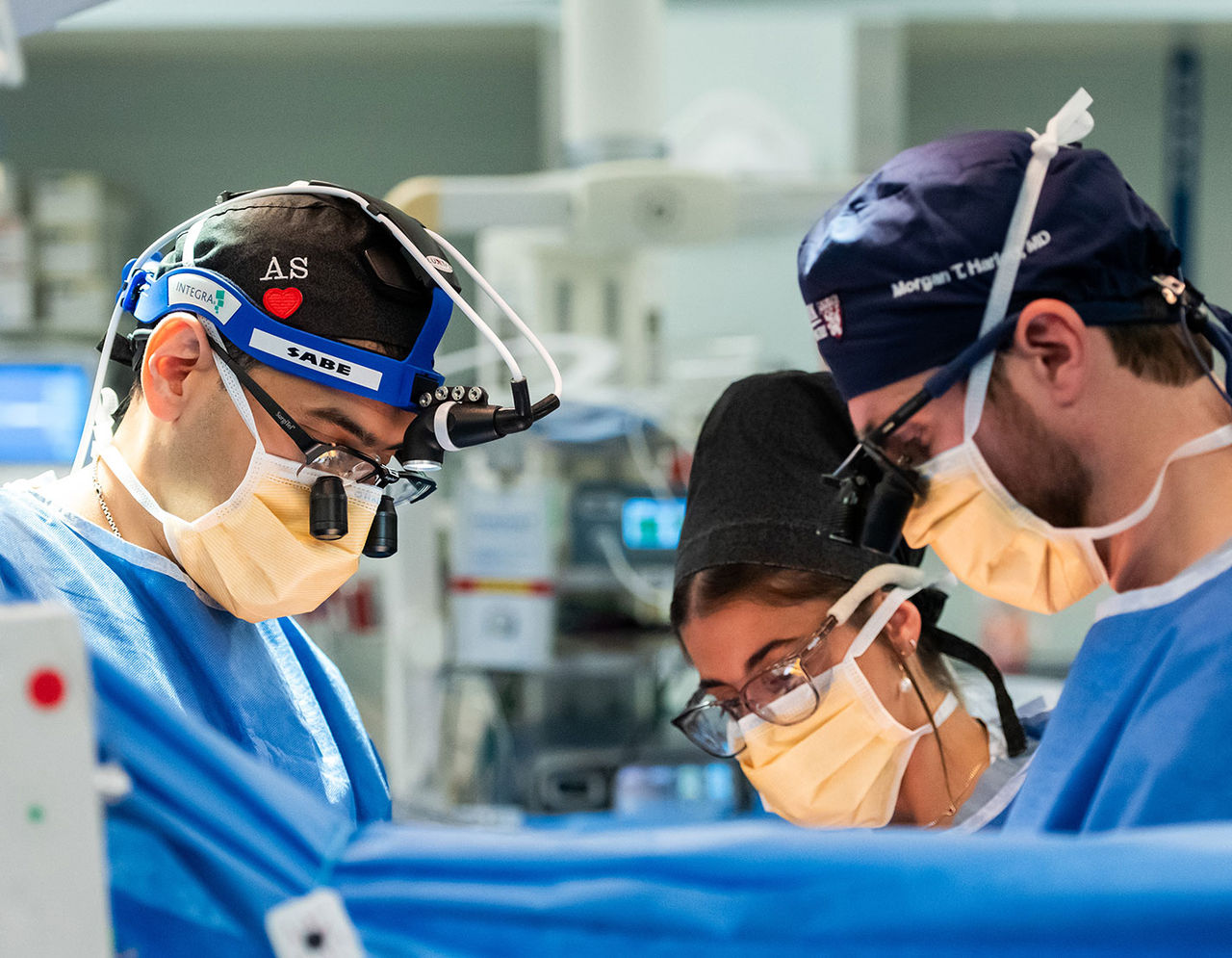
If the hole is large enough or does not close on its own, heart surgery may be required for ASD repair or closure. The surgery may be performed robotically, or a surgeon will cut an incision into the chest and directly patch the hole in the heart. This may be the only option for patients with ostium primum, sinus venosus, and coronary sinus.
If heart surgery is needed, a three or four-day stay in the hospital is generally required for recovery. Once home, activities will be limited. The chest incision should heal within six weeks.
How to live with atrial septal defect
Anyone with a history of atrial septal defect will need to remain under the care of a cardiologist to monitor for any complications. Patients with hole in heart can expect to live a healthy life.
An echocardiography may be needed every two to three years to evaluate heart function and structure. Typically, if someone has been treated with catheterization or heart surgery, no further procedures or surgeries are needed.
If there is only a small hole in the heart or you've been successfully treated for ASD, normal activities can be enjoyed unless your physician instructs otherwise. Restrictions in activity are usually only prescribed after a procedure or surgery, and normal activities can be resumed once recovery is complete.
FAQs
Atrial septal defects can often close on their own. If a hole in the heart does not close on its own, or if the opening is too large, procedures or heart surgery may be needed for an atrial septal repair.
If treated, someone with atrial septal defect can expect a normal life expectancy. However, if left untreated, evidence suggests your life expectancy could be shortened due to a higher risk of heart failure or stroke.
If an atrial septal defect does not close on its own, then a cardiologist will advise when the ASD should be closed.
It is possible to live your entire life without experiencing any symptoms from ASD or even knowing of its presence. However, once you are diagnosed, a physician will decide how much and how frequently to monitor the condition and if medications, nonsurgical, or surgical procedures are necessary.
Atrial septal defect is one of the most common congenital heart defects, affecting about 25% of children. ASD can sometimes go undetected and undiagnosed until adulthood.