-
- Find Care
-
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
-
-
-
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
- Participate in Research
-
- Contact us
-
- For Innovators
- Commercialization Guide for Innovators
-
-
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Getting Started
- New to Mass General Brigham
- International Patient Services
- What Is Patient Gateway?
- Planning Your Visit
- Find a Doctor (opens link in new tab)
- Appointments
- Patient Resources
- Health & Wellness
- Flu, COVID-19, & RSV
- Billing & Insurance
- Financial Assistance
- Medicare and MassHealth ACOs
- Participate in Research
- Educational Resources
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
- Find Care
-
- Overview
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
-
- Overview
- Participate in Research
-
- Overview
- About Innovation
- About
- Team
- News
- For Industry
- Venture Capital and Investments
- World Medical Innovation Forum (opens link in new tab)
- Featured Licensing Opportunities
- For Innovators
- Commercialization Guide for Innovators
- Contact us
-
- Overview
- Information for Researchers
- Compliance Office
- Research Cores
- Clinical Trials
- Advisory Services
- Featured Research
- Two Centuries of Breakthroughs
- Advances in Motion (opens link in new tab)
- Brigham on a Mission (opens link in new tab)
- Gene and Cell Therapy Institute
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Residency & fellowship programs
- Brigham and Women's Hospital
- Massachusetts General Hospital
- Mass Eye and Ear
- Newton-Wellesley Hospital
- Salem Hospital
- Integrated Mass General Brigham Programs
- Centers of Expertise
- Global & Community Health
- Health Policy & Management
- Healthcare Quality & Patient Safey
- Medical Education
- For trainees
- Prospective trainees
- Incoming trainees
- Current trainees
- Continuing Professional Development
Jenn’s Story: From Brain Surgery to Hiking the Alps
In May 2022, Jenn Murff, PhD, MA, had just spoken at a conference in Sweden. As she stepped off the stage, she was suddenly struck by the worst headache of her life. She had never felt anything like it before: a squeezing, tight pressure that left her in agony.
As the CEO of an international Christian ministries organization and a busy mom of four daughters, she initially brushed aside her pain.
“I figured it was a migraine. You don’t need to go to the hospital for a migraine,” she says.
But the terrible pain lingered even after she returned home to Virginia. Eventually, she went to the hospital, where she was shocked to learn she had a severe brain condition called arteriovenous malformation, or AVM, which is sometimes fatal.
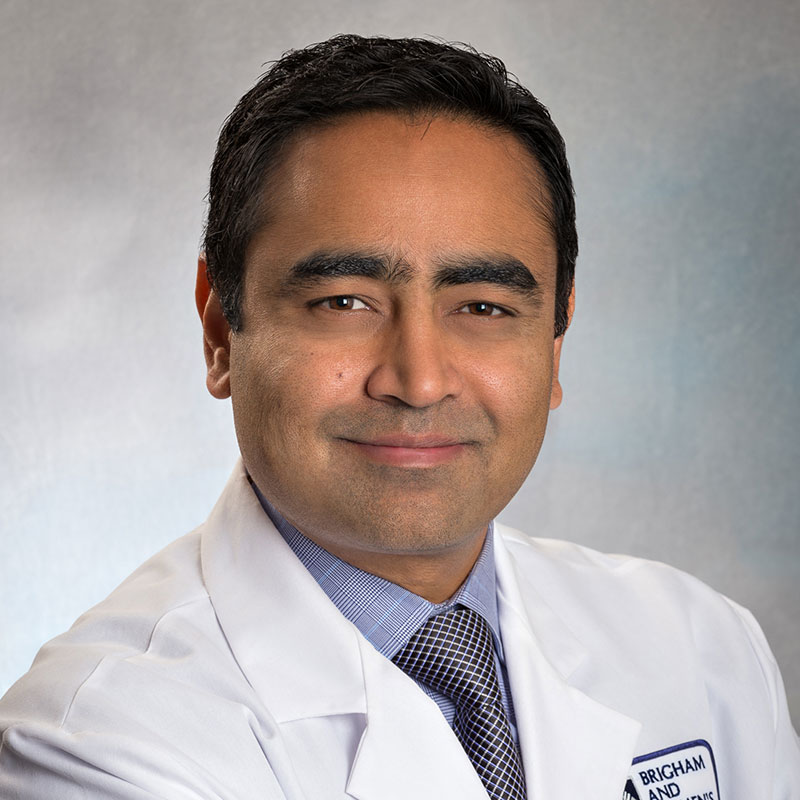
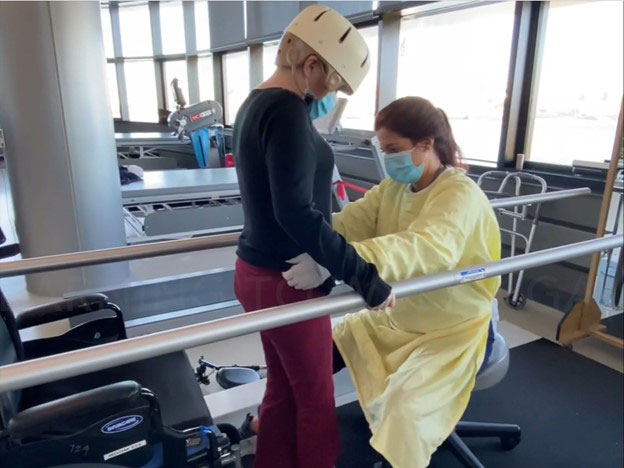
Nirav Patel, MD, a Mass General Brigham neurosurgeon, is the director of the AVM Program at Brigham and Women’s Hospital. He is known worldwide for treating the most complex AVMs. Dr. Patel and his team were able to remove Jenn's AVM in a long but successful surgery. Jenn then worked with Rebecca Phelan, DPT, a Mass General Brigham physical therapist at Spaulding Rehabilitation, to complete her recovery. Thanks to their dedicated care and her own determination, Jenn would dodge disaster and return to the life she loves.
AVM diagnosis and treatment
Surgery for AVM: A complicated, delicate procedure
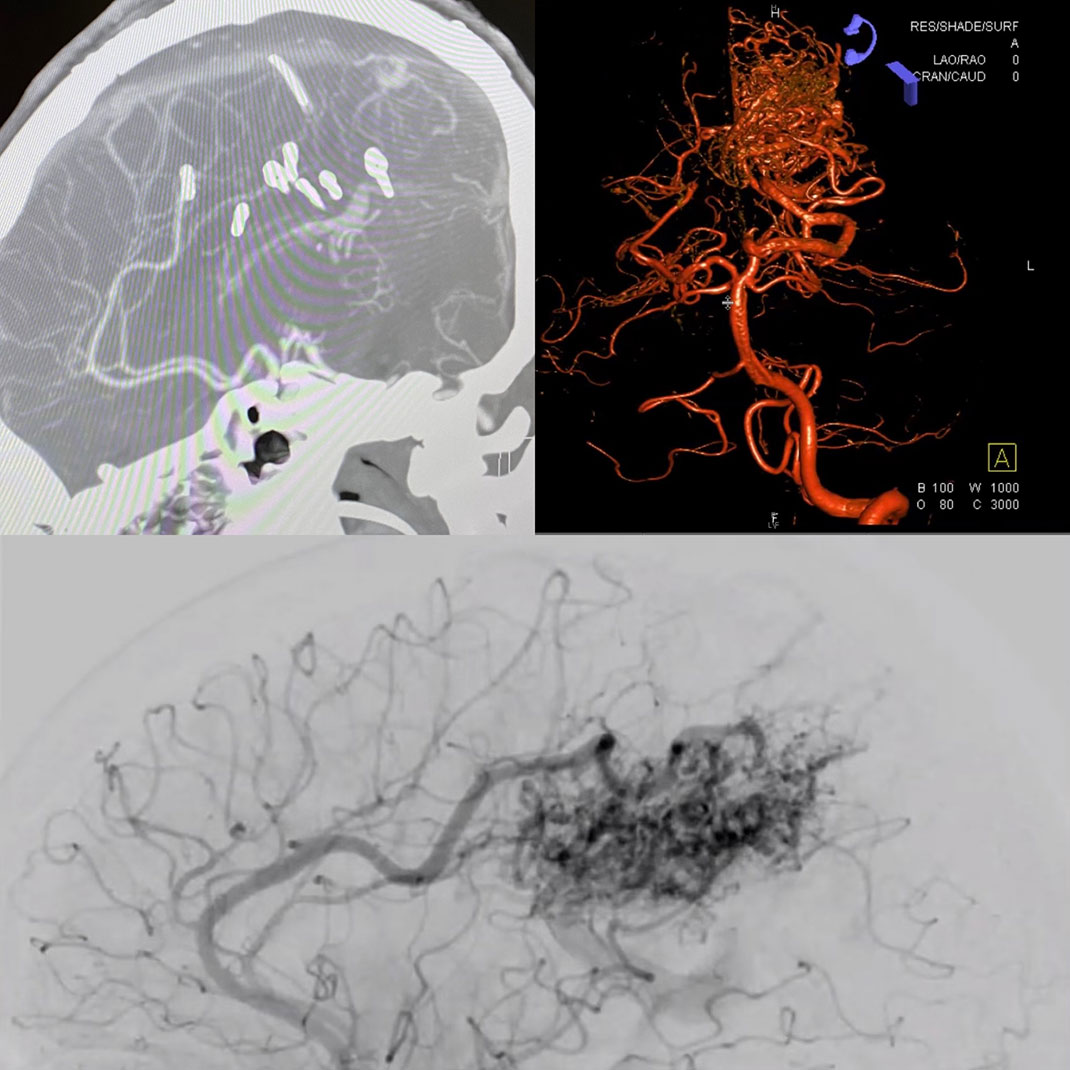
AVM surgeries are complex, delicate procedures neurosurgeons perform under a microscope for greater precision. Neurosurgeons untangle the malformed blood vessels and slowly remove them, one millimeter at a time.
A multidisciplinary team works together to provide care. While the surgical team works in the operating room, other providers monitor progress through an angiogram. Angiograms are special tests that show blood flowing through arteries and veins in real time. This allows the surgeon to adjust course and protect delicate structures of the brain.
Dr. Patel knew that Jenn’s AVM surgery would be difficult. She would also face a long and challenging recovery after the surgery was complete.
“Whenever I see an AVM, the first question I ask myself is: Can I do this? Am I physically capable? If the answer is yes, the second question I ask myself is, should I do this? And the ‘should’ is wrapped up in the other person — the patient. I told Jenn this was going to be a very difficult operation with a high risk for lasting complications,” Dr. Patel explains.
Jenn felt confident in Dr. Patel and the Mass General Brigham team, and decided to go ahead with the surgery.
Personalized AVM care
Mid-sized AVMs can take 12 hours to remove. Jennifer’s was so complex and spread so deeply throughout her brain that it took more than twice that time. Dr. Patel and his team performed 3 individual surgeries over 7 days. Jennifer remained sedated in the Intensive Care Unit (ICU) between each procedure, under constant monitoring from a dedicated nursing team.
During Jenn’s operation, Mitali Bose, MS, CNIM, a Mass General Brigham neuro-physiologist, assisted Dr. Patel. “Neuromonitoring doesn’t take away all risk, but it gives the surgeon a lot more confidence,” says Dr. Patel.
By the end of the third surgery, the team was satisfied Dr. Patel had completely removed the AVM. While the surgeries had taken an enormous toll on her brain — impacting her ability to walk and talk — Jenn was finally ready to heal.
Physical rehabilitation after AVM surgery